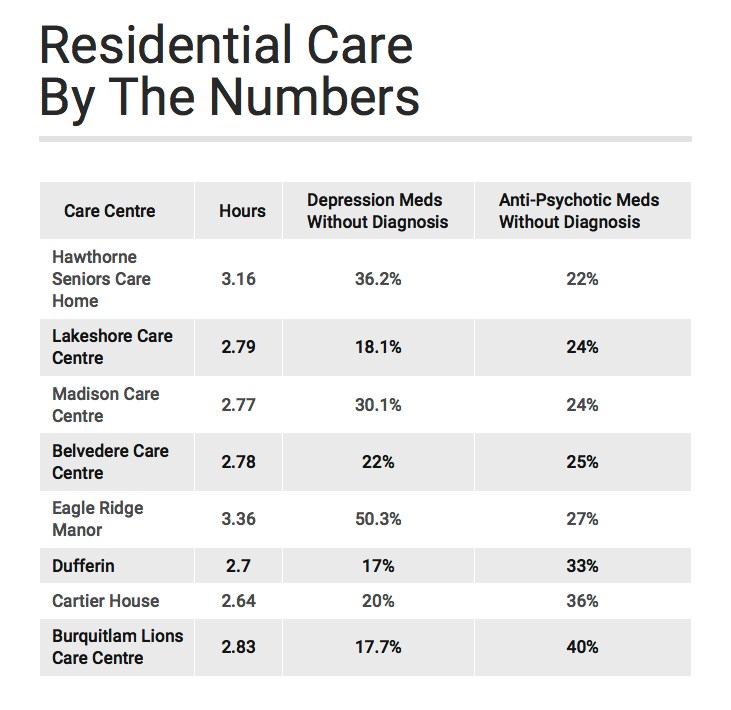
A new directory of residential care facilities — including several Tri-City senior care homes — shows widespread prescription of anti-depression and anti-psychosis drugs for people who haven't been diagnosed with the illnesses and care levels below recommended guidelines.
"A lot were caught by surprise — I know I was," Isobel Mackenzie, B.C. Seniors Advocate
And the seniors advocate who released the B.C. Residential Care Quick Facts Directory last week says she hopes the alarming data is a wake-up call to policy makers and health care providers.
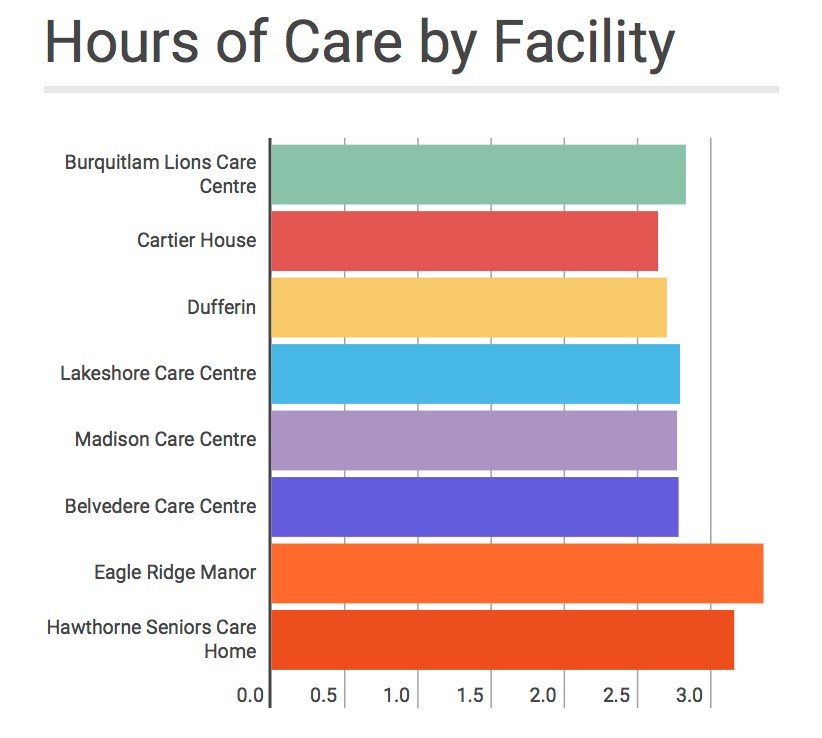
"A lot were caught by surprise — I know I was," said the advocate, Isobel Mackenzie, who said she hopes the data that shows 80% of facilities don't meet the Ministry of Health guidelines for 3.36 hours of daily care per resident will help families advocate for their loved ones and prompt changes in the sector.

"It's only a guideline and, in fact, people aren't meeting it means maybe we need to have something firmer than a guideline," Mackenzie said.
Health Minister Terry Lake has also seen the data and now says he wants a review.
LESS CARE
In the Tri-Cities, for example, only Eagle Ridge Manor, which is located on the grounds of Eagle Ridge Hospital and is run by Fraser Health, meets the recommended hours of care, with the remaining seven local facilities ranging from a low of 2.64 hours at Cartier House in Coquitlam to a high of 3.16 hours at Hawthorne Seniors Care home in Port Coquitlam.
The hours reflect the time nurses spend helping residents with daily tasks as well as programs and therapies such as recreation and physiotherapy. The numbers are determined by the contract and funding, not by the facility managers or owners, Mackenzie said.
The prescription of depression medication and antipsychotic drugs has also become an issue.
Mackenzie said antipsychotic drugs might calm agitated people but may also make them more lethargic. Depression medicine may be overly prescribed, too, and she wants to know if there's a link between their use and staffing levels.
"We don't know that, yet," Mackenzie said, noting, "You aren't seeing higher use in facilities where the population has a higher level of aggressive behaviour, that's not showing."
And while B.C.'s rates of prescribing these drugs are trending downward this year, they are still higher than those in many other provinces, Mackenzie said.
POWERFUL DRUGS
In B.C., for example, 47.8% of care home residents are given depression medicine but only 24% are actually diagnosed with depression.
And 31% of residents are given antipsychotics without a diagnosis of psychosis. The actual rate of psychosis among the elderly is about 4%, "so the number is actually higher," she said.
In the Tri-Cities, the use of powerful antipsychotic drugs for uses other than those approved by Health Canada varies depending on the facility, however, Mackenzie said she thinks the medications are being over-prescribed and she wants to know why.
"It should be rare or temporary to administer Ativan [and anti-anxiety drug] and Haldol [an anti-psychotic] because the situation is acute and you should be trying a number of things before you do it. I think the evidence is we're not doing that," said Mackenzie.
"We know there is still work to do," Tasleem Juma, Fraser Health spokesperson
Fraser Health, meanwhile, is taking these issues seriously, said a spokesperson, and is working on improvements to drug prescription protocol and ensuring facilities run by the authority meet the recommended hours of care.
MORE WORK
"We know there is still work to do," said Fraser Health's Tasleem Juma, but she noted the health authority regularly consults with providers to ensure they have enough resources and ensures all of Fraser Health-owned and -operated facilities meet the direct care guidelines.
For example, two facilities opening this month in the Tri-Cities — Foyer Maillard, which will have 80 new residential complex care beds, and Baltic Properties, with 160 beds — will be funded to the recommended number of care hours, Juma said.
She also said the direct care hours are only one measure of livability because care homes also have special recreation programs, amenities and gardens that make them pleasant for residents.
As for the over-prescribing of anti-depression and anti-psychotic drugs, Juma said, a study into their use was initiated two years ago and two care facilities, one in Mission and one in Burnaby, are piloting a new protocol that would see more people, including family members, consulted before drugs are prescribed.
HIGH EXPECTATIONS
Mackenzie wonders if changing the culture is needed as well to convince people, including well-meaning family members, not to prescribe a pill for every ailment. She said the requirement that everyone be happy all the time might be unrealistic objective, especially for frail seniors.
"It may be not unreasonable that someone is a little glum, especially when they move [from their home into a care facility]. I think we are rushing too quickly to medicate," she said.
At the very least, she said she hopes the directory will provide food for thought and a basis for further research.



