Police need help to diffuse and resolve mental health crises safely, say Tri-City politicians, who would like to see trained professionals assisting Port Moody police and Coquitlam RCMP in some emergency calls.
With mental health calls to Coquitlam RCMP climbing, a special police car could be sent to deal with some situations where people are at risk of harming themselves or others, the politicians say.
School District 43 trustees are calling for Fraser Health to work with Port Moody police and Coquitlam RCMP to establish a mental health car, which would go out on some calls, as is the case in Surrey and Vancouver, and many other cities.
In calling for the initiative at their June 16 meeting, trustees acknowledged that mental health has become an urgent issue, particularly during the COVID-19 pandemic.
Specialized training
“When parents are struggling the only solution is to call 911 and hope the person on the other end of the line is trained,” said Port Coquitlam trustee Michael Thomas.
Port Moody and Coquitlam RCMP have officers with specialized training but they aren’t always available to go out on calls with general duty officers.

Coquitlam Mayor Richard Stewart said he supports the trustees’ request, adding he’s made similar entreaties to Fraser Health in the past because he thinks police are not well-equipped to deal with someone in mental health crisis.
“We really need Fraser Health to step up and partner with police forces on a regional level and figure this out so we can deliver better service that’s more appropriate to the need of the psychiatric crisis patient. A psychiatric patient doesn’t need a bullet proof vest and a gun,” Stewart said.
In a potentially dangerous situation, mental health workers could provide psychiatric assessment while police, who are trained in de-escalation, could ensure everyone is safe, Stewart said.
He also noted that police don’t have the resources to sit for hours at Royal Columbian Hospital waiting for a doctor to help someone who has been apprehended under the Mental Health Act.
“It’s something that I’ve raised in the past. The way to get into the mental health system in B.C.. Is through the hospital emergency ward and the way to get to it for so many people is by calling 911 and the ambulance doesn’t come, it’s the police who come.”
Stewart’s concerns echo those made recently by the Canadian Mental Health Association and others calling for specially-trained mental health units and more funding for mental health.
A national issue
Calls for additional resources to support police in handling mental health crisis calls comes as the head of RCMP’s Southeast District in B.C. says he wants to add more mental health teams in the region, in the wake of a disturbing video of a police wellness check in which a young woman was dragged down a hallway.
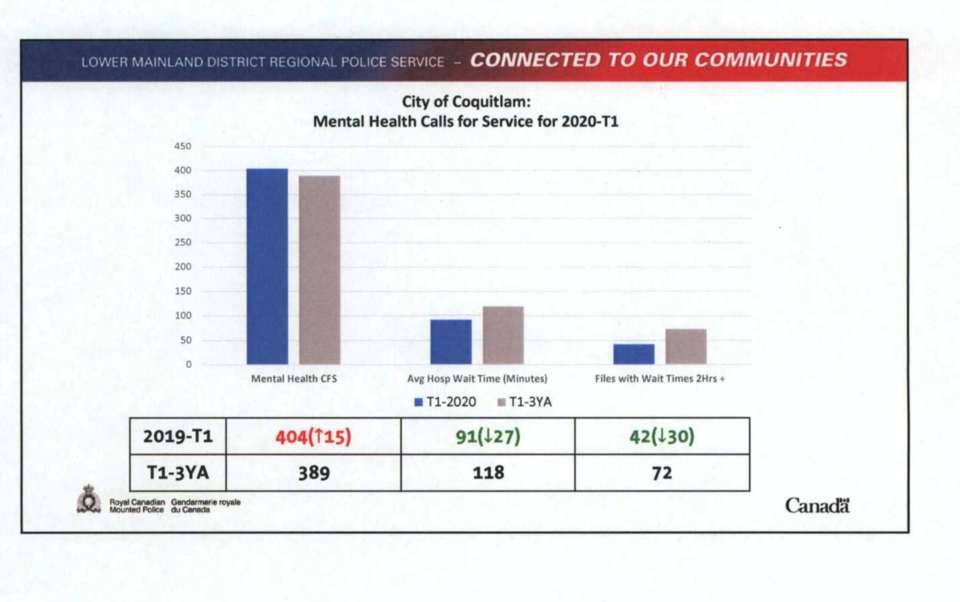
In Coquitlam, RCMP handled 404 mental health calls for service in the first three months of the year, up from a three-year average of 389, and the average wait time in hospital with a patient is 90 minutes.



